What are mitochondrial disorders?
- Mitochondrial disorders are a clinically heterogeneous group of disorders that arise as a result of dysfunction of the mitochondrial respiratory chain1
- The estimated prevalence of mitochondrial disorders was found to be at least 20 per 100,000 in the population2
Types of mitochondrial disorders
Common clinical features of mitochondrial disorders include ptosis, external ophthalmoplegia, proximal myopathy and exercise intolerance, cardiomyopathy, sensorineural deafness, optic atrophy, pigmentary retinopathy and diabetes mellitus.1
Mitochondrial disorders and their primary clinical features:1
| Mitochondrial disorder | Primary clinical features |
| Alpers-Huttenlocher syndrome |
|
| ANS (including SANDO and MEMSA*) |
|
| CPEO |
|
| KSS |
|
| Pearson syndrome |
|
| LIMM (fatal and non-fatal forms) |
|
| Leigh syndrome |
|
| NARP |
|
| MELAS |
|
| MEMSA* |
|
| MERRF |
|
| LHON |
|
Overlapping and differentiating symptoms of mitochondrial disorders and AADC deficiency
- In infants, clinical features such as hypokinetic rigid syndrome and generalised dystonia can mimic those seen in AADC deficiency and other paediatric neurotransmitter disorders, making diagnosis difficult based on clinical presentation alone3
- The presence of oculogyric crises may help to differentiate AADC deficiency from a mitochondrial disorder, however, this is not sufficient to make a definitive diagnosis as although it is not typical, oculogyric crises may sometimes present in mitochondrial disorders4
- Therefore, molecular genetic testing is warranted to confirm or rule out a diagnosis of AADC deficiency5
Overlapping and differentiating symptoms of mitochondrial disorders and AADC deficiency:
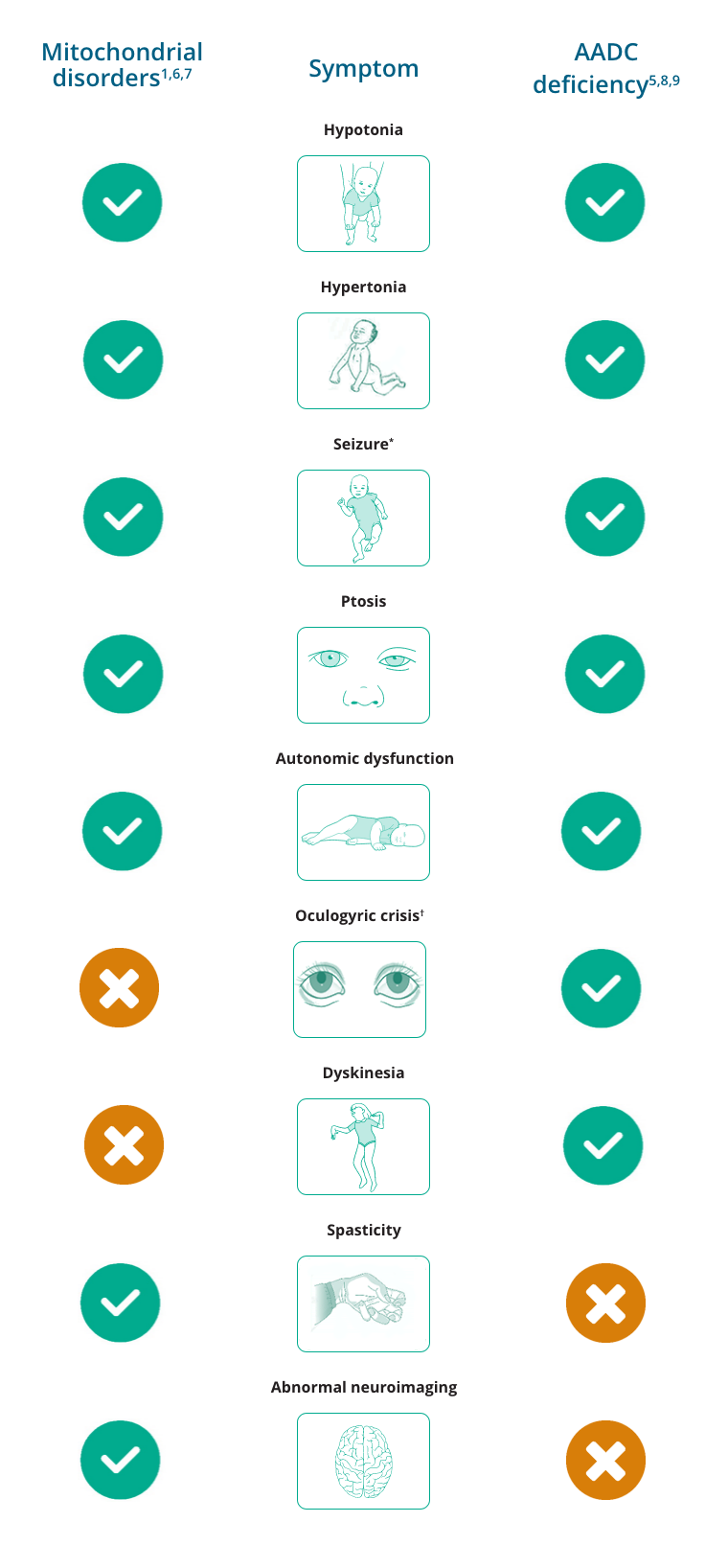
*Seizures are uncommon in AADC deficiency but have been reported.
†While oculogyric crisis has been reported, it is not typical of mitochondrial disorders.
- Adam MP, Ardinger HH, Pagon RA, et al (Editors). GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993–2020.
- Schaefer AM, et al. BBA. 2004;1659:115–120.
- Marecos C, Ng J, Kurian MA. J Inherit Metab Dis. 2014;37:619–626.
- Garcia-Cazorla A, et al. Mitochondrion. 2008;8:273–278.
- Wassenberg T, et al. Orphanet J Rare Dis. 2017;12:12.
- Garcia-Cazorla A, et al. Mitochondrion. 2008;8:273–278.
- Ng J, et al. Nat Rev Neurol. 2015;11:567–584.
- Manegold C, et al. J Inherit Metab Dis. 2009;32:371–380.
- Gropman AL. Neurotherapeutics. 2013;10:273–285.
Explore interactive clinical case studies
