Summary of AADC deficiency
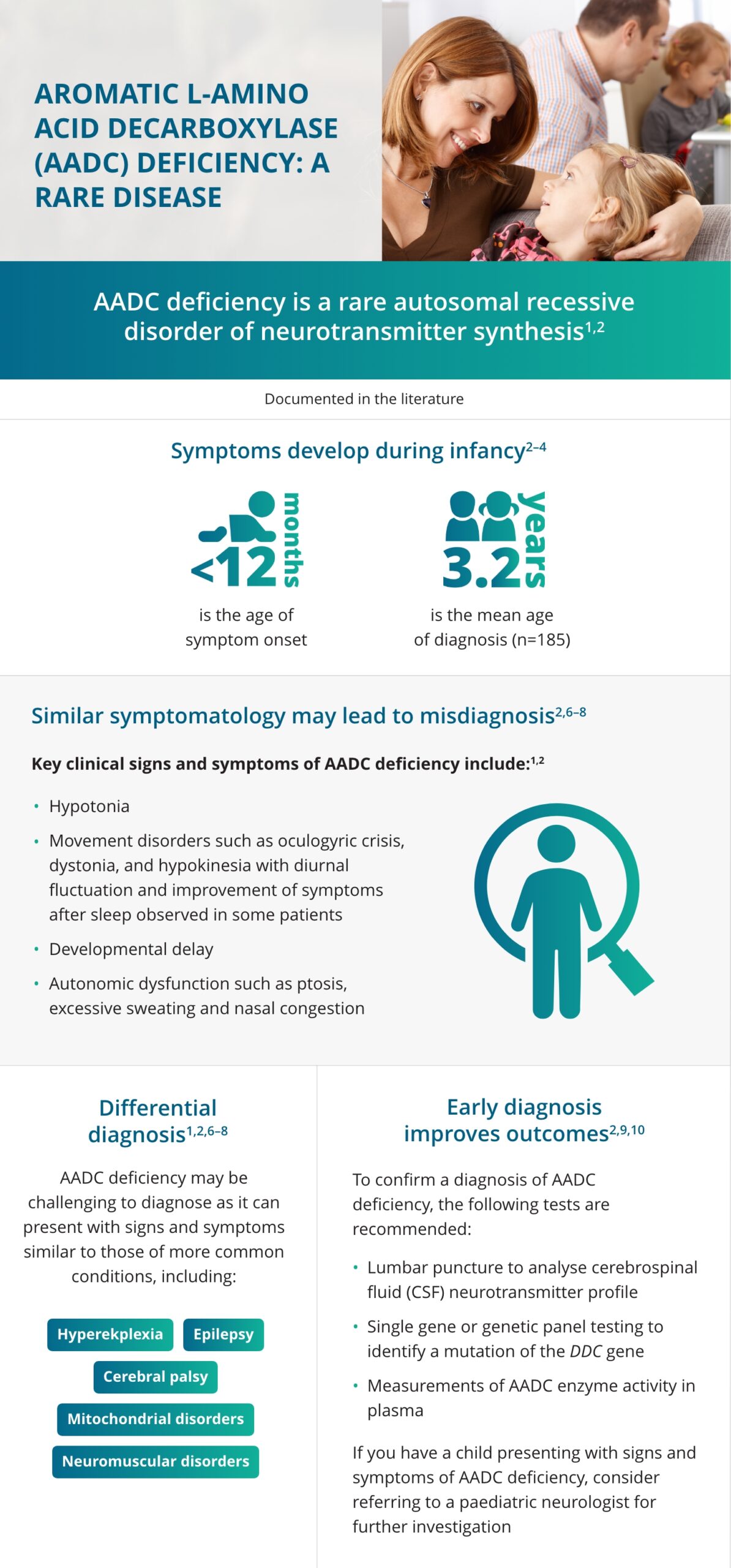
Aromatic L-amino acid decarboxylase (AADC) deficiency is a rare, genetic disease.1,2 A mutation in the DDC gene results in reduced activity of the AADC enzyme.1,2 The AADC enzyme plays an important role in producing the key neurotransmitters, dopamine and serotonin.2
In AADC deficiency, the reduction of these neurotransmitters causes the associated symptoms, such as hypotonia, movement disorders, developmental delay and autonomic symptoms.2 Symptom onset occurs during infancy, but mean diagnosis is typically delayed until 3.2 (±5.7) years.2–4
Animation: Signs and symptoms of AADC deficiency
Watch this short animation to learn more about the biochemical basis of AADC deficiency, the commonly observed symptoms and the guideline-recommended tests for definitive diagnosis.
Aromatic L-amino acid decarboxylase deficiency or AADC deficiency is a rare inherited disorder of neurotransmitter synthesis resulting from a mutation in the dopa decarboxylase or DDC gene. Mutations in the DDC gene result in a significant reduction or complete loss of AADC enzyme activity, leading to a deficiency of dopamine, neurotransmitters, epinephrine and serotonin.
These changes lead to symptoms first appearing around 3 months and affect neuronal signalling in the central nervous system, which is required for motor and behavioural development and autonomic function. Symptoms may vary from patient to patient. But the most common symptoms include: developmental and motor delay, hypotonia, oculogyric crisis, akinesia, dystonia, and autonomic dysfunction, which do not typically improve over time leading to the need for lifelong care.
These symptoms overlap with those seen in other conditions such as cerebral palsy, epilepsy and neuromuscular conditions, which can mean that cases of AADC deficiency are challenging to differentially diagnose or can go undiagnosed.
Earlier identification can help improve the care and management of patients. One or more of the following red flag diagnostic signs should prompt referral to a paediatric neurologist and investigation for a neurotransmitter disorder: oculogyric crisis, hypotonia, developmental delay, lack of abnormalities in neuroimaging, multiple features of autonomic dysfunction.
Once your patient has been seen by a paediatric neurologist, they can undergo three possible core diagnostic tests to identify or confirm an AADC deficiency diagnosis. These include a CSF neurotransmitter metabolite panel and/or plasma AADC enzyme activity assay in combination with the genetic testing to confirm a diagnosis of AADC deficiency.
Earlier identification of the distinguishing signs and symptoms of AADC deficiency may help improve patient care and outcomes, please visit the diagnosis & testing page of the www.aadcinsights.eu website.
In focus: Signs and symptoms of AADC deficiency2
 Hypotonia
Hypotonia
Children with AADC deficiency commonly have hypotonia with poor head control
 Developmental delay
Developmental delay
Children often have delayed motor, cognitive and speech development
 Movement disorders
Movement disorders
The most common movement disorder in AADC deficiency is oculogyric crises, but dyskinesia, dystonia, hypokinesia, tremors and myoclonus can be present
 Oculogyric crises5
Oculogyric crises5
An involuntary upward deviation of the eyes that are often mistaken for seizures
 Autonomic dysfunction
Autonomic dysfunction
Multiple symptoms associated with the autonomic nervous system such as nasal congestion, excessive drooling, temperature instability
Infographic: Signs and symptoms of AADC deficiency
Despite early symptoms appearing in infancy, diagnosis is delayed with a mean diagnostic age of 3.2 (±5.7) years.2–4 This is often because symptoms of AADC deficiency overlap with other more common conditions such as epilepsy or cerebral palsy, leading to potential misdiagnosis.6 Identifying AADC deficiency symptoms and carrying out appropriate diagnostic tests can help to ensure early diagnosis and improve outcomes for patients and their caregivers.2,5–7
Access exclusive expert-led educational content
- Access on-demand presentation content delivered by world-renowned experts in the field of neurotransmitter disorders
- Attend and access content from exclusive educational events for healthcare professionals involved in the referral, testing, diagnosis and management of patients with these conditions
- Engage with peers from around the world to help improve clinical practice and patient care in neurotransmitter disorders
Learn more about the differential diagnoses of AADCd
- Brun L, et al. Neurology. 2010;75:64–71.
- Wassenberg T, et al. Orphanet J Rare Dis. 2017;12:12.
- Rizzi S, et al. Behav Neurol. 2022;2022:2210555.
- Bergkvist M, et al. Future Neurol. 2022;17(4):FNL63.
- Lee WT. Epilepsy & Seizure. 2010;3(1):147–153.
- Ng J, et al. Nat Rev Neurol. 2015;11(10):567–584.
- Krigger KW. Am Fam Physician. 2006;73(1):91–100.
- Pons R, et al. Neurology. 2004;62:1058–1065.
- Himmelreich N, et al. Mol Genet Metab. 2019;127(1):12–22.
- National Organization for Rare Diseases. AADC deficiency. Available from: https://rarediseases.org/rare-diseases/aromatic-l-amino-acid-decarboxylase-deficiency. Accessed March 2024.
