Symptoms and impact of aromatic L–amino acid decarboxylase (AADC) deficiency: A qualitative study and the development of a patient–centred conceptual model
Williams K, et al. Curr Med Res Opin. 2021; Online ahead of print.
Publication Date | June 2021
Authors | Williams K, Skrobanski H, Werner C, O’Neill S, Buesch K and Acaster S
Citation | Curr Med Res Opin. 2021; Online ahead of print; DOI: 10.1080/03007995.2021.1932449
https://pubmed.ncbi.nlm.nih.gov/34042550/
The symptoms of aromatic L-amino acid decarboxylase (AADC) deficiency are documented in the literature1–4 but limited research has been conducted with patients or their caregivers, and qualitative research studies exploring the impact of disease are particularly lacking. The aim of the study conducted by Kate Williams et al was to explore the symptoms, functional impairment and disease impact experienced by individuals with AADC deficiency from the caregiver perspective.1
Participants had to be the main caregiver (providing at least 50% of daily care) of individuals with an AADC deficiency diagnosis confirmed by cerebrospinal fluid (CSF) neurotransmitter analysis, molecular genetic testing of the DDC gene, and/or blood AADC enzyme activity, aged 18 years or over, living in the United States, Canada, United Kingdom, France, Italy, Spain or Portugal, and were willing and able to provide informed consent.1 Interviews were conducted with participants via telephone or video conference.1
Interviews were conducted with 14 caregivers of 13 individuals with AADC deficiency.1 Most individuals were completely dependent on their caregivers for all aspects of their lives.1 The overall symptoms, functional impairment and daily-life impact on individuals with AADC deficiency reported by their caregivers are illustrated in the conceptual model in Figure 1.1
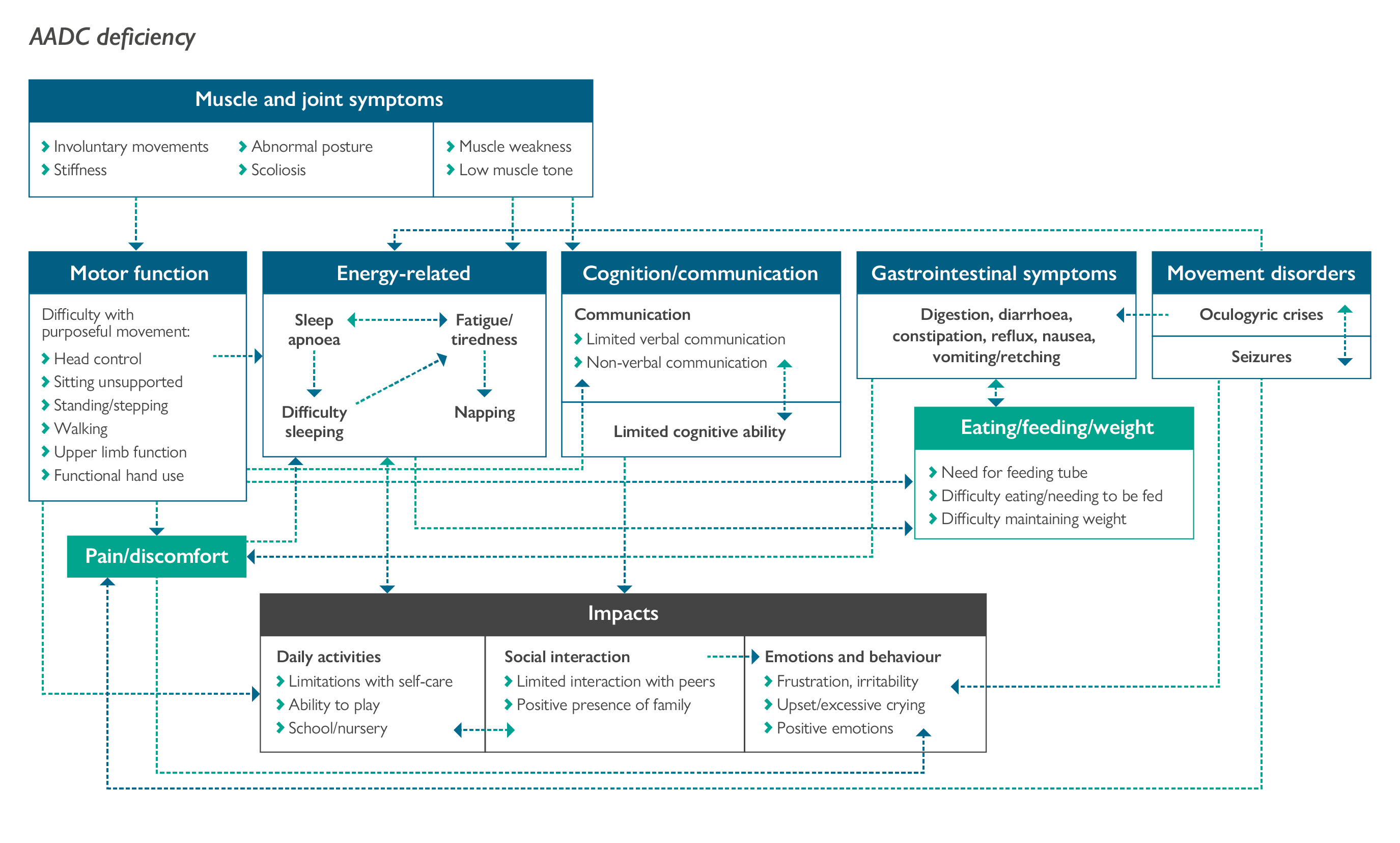
Nearly all caregivers stated the individual they care for had muscle and joint symptoms, particularly muscle weakness and low muscle tone, that limited their motor function, including their ability to hold their head up, sit unsupported, stand, walk and use their upper limbs.1 Only approximately half of the caregivers reported that the individual with AADC deficiency was able to control their head and hold it level, and fewer than half reported that the individual was able to sit unsupported.1 Less than a third of caregivers reported that the individual had some ability to walk short distances with minimal or no support.1 The majority of caregivers reported that the individual experienced episodes of oculogyric crises, often affecting the whole body, and included characteristics such as eyes rolling back in the head, staring upwards, stiffness, shivering, pain and involuntary movements.1
The majority of caregivers reported that the individual with AADC deficiency experienced difficulty getting to sleep, fatigue and tiredness, attributed to muscle weakness and motor function impairment.1 Several caregivers reported the presence of sleep apnoea and around half of the individuals with AADC deficiency required ventilation at night to support their breathing.1
Most caregivers described the individual’s cognitive function as extremely limited to just recognising objects, sounds and people, but varied depending on whether they were having ‘a good day’ or ‘a bad day’.1 Similarly, the individual’s ability to communicate varied from day to day, but was overall limited to sounds, use of eye movements, facial expressions, or body gestures (e.g. tapping) to communicate.1
Most caregivers reported that the individual with AADC deficiency experienced difficulties with food consumption and/or gastrointestinal symptoms, including problems with digesting food, diarrhoea, constipation, reflux, nausea and vomiting.1 Consequently, several reported that the individuals they cared for ate through a feeding tube to avoid gastrointestinal issues and to ensure they got enough nutrients to help them maintain their weight.1
The symptoms and functional impairments reported by caregivers had a wider impact on the individual’s daily activities and quality of life.1 Around half of the individuals with AADC deficiency attended school or nursery.1 All caregivers stated the individual was unable to do any of the usual activities of other children their age and the limited function had a negative impact on their ability to do leisure activities and socialise with their peers, affecting their emotional wellbeing.1
The results from this qualitative research study add to our understanding of the symptoms, challenges and subsequent burden of living with AADC deficiency, for both the individual with AADC and their caregiver. Individuals with AADC deficiency experience a range of physical and emotional symptoms that have a substantial impact on their daily life and result in the need for 24-hour care or support from a caregiver.1 The patient-centred conceptual model proposed by the authors illustrates how the symptoms, functional impairments and impacts experienced by individuals are interrelated.1 The authors suggest treatments that improve function and symptoms have the potential to improve the daily lives and health-related quality of life of these individuals.
- Williams K, Skrobanski H, Werner C, et al. Curr Med Res Opin. 2021;Online ahead of print.
- Wassenberg T, Molero-Luis M, Jeltsch K, et al. Orphanet J Rare Dis. 2017;12:12.
- Pearson TS, Gilbert L, Opladen T, et al. J Inherit Metab Dis. 2020;43:1121–1130.
- Brun L, Ngu LH, Keng WT, et al. Neurology. 2010;75:64–71.
