What is cerebral palsy?
- Cerebral palsy (CP) is a group of permanent neuromotor disorders causing activity limitations attributed to non-progressive disturbances that occurred in the developing foetal or infant brain, accompanied by developmental delay1,2
- It is the most common cause of severe physical disability in children, with a prevalence of 1.7–3.1 per 1,000 live births in high-income countries, and a higher prevalence in low-income countries3
Classification of cerebral palsy
There are several forms of CP, classified according to which part of the central nervous system is malformed or damaged and the different manifestations.4,5
Spastic CP
- Spastic CP is the most common form of the condition, representing >70% of cases. Symptoms include stiff, spastic muscles, abnormal movements, difficulties controlling and coordinating muscle movements, and impairment of oral, lingual and palatal movement, which results in dysarthria and dysphagia. Consequently, patients fail to reach normal milestones for sitting, crawling and walking4,5
Athetoid or dyskinetic CP
- Athetoid or dyskinetic CP occurs in ~20% of cases and is characterised by slow, writhing movements (athetosis), repetitive, twisting motions (dystonia), and unpredictable, irregular movements (chorea). These abnormal motions can all range from slow to rapid and can be accompanied by pain. Movements may increase with emotional tension and may disappear during sleep‡4,5
Ataxic CP
- Ataxic CP occurs in less than 5% of cases. Symptoms include weakness, poor coordination, tremors and shaky movements, unsteadiness and balance problems, and difficulty with rapid or fine movement4,5
Mixed CP
- Mixed CP is a common occurrence whereby patients present with a combination of symptoms. It generally includes spasticity and athetosis4,5
Overlapping and differentiating symptoms of cerebral palsy and AADC deficiency
- Many of the childhood manifestations of CP are similar to those seen in patients with a monoamine neurotransmitter disorder such as AADC deficiency6
- Consequentially, the term ‘CP mimic’ is used to describe a number of neurological disorders that manifest similarly in early childhood2
- Clinical symptoms of AADC deficiency that are atypical in CP include oculogyric crises and diurnal variation of motor symptoms
- Appropriate investigations, including analysis of neurotransmitters in cerebrospinal fluid, are essential for an accurate clinical diagnosis2,7
- CP mimics also show several features that differ from classic CP and can serve as diagnostic clues, including multiple features of autonomic dysfunction
- Features of autonomic dysfunction include excessive sweating (diaphoresis), temperature instability, profuse nasal and oropharyngeal secretions, poor gut movements (gastrointestinal dysmotility) and sleep disturbances2
Overlapping and differentiating symptoms of CP and AADC deficiency:*
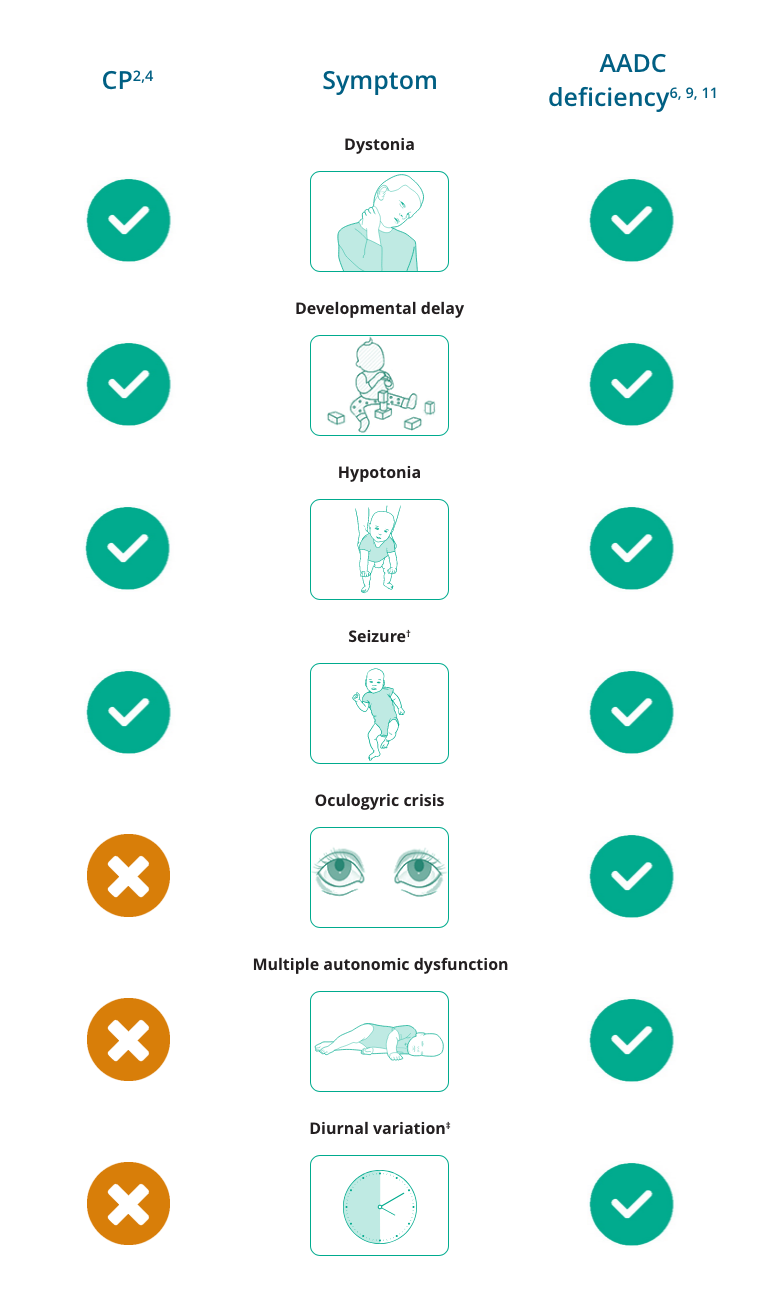
*Not an exhaustive list.
†Seizures are relatively uncommon in CP and are uncommon in AADC deficiency, but have been reported in both. Seizures in CP have been reported primarily to be of a generalised or partial subtype.12,13
‡Diurnal variation is not always a feature of AADC deficiency but is consistently reported.11
Workup of patients with cerebral palsy symptoms
- Brain MRI is a first‐line investigation in a child or adult with an undiagnosed motor disorder which suggests CP2
- Brain imaging can readily reveal a cerebral malformation as the main cause of neurological symptoms2
- Aside from cerebral malformation, brain imaging can reveal either normal findings or specific lesions which are characteristic of a genetic disorder or group of disorders, which should prompt further investigation2
-
- Novak I, et al. JAMA Pediatrician. 2017;171:897–907.
- Pearson TS, et al. Mov Disord. 2019;34:625–636.
- Monbaliu E, et al. Lancet Neurol. 2017;16: 741–749.
- Cerebral Palsy Guidance. Cerebral Palsy Symptoms. Available from: https://www.cerebralpalsyguidance.com/cerebral-palsy/symptoms/. Accessed April 2022.
- Cerebral Palsy (CP) Syndromes (n.d.). Merck Manuals Professional Edition. Available from: https://www.merckmanuals.com/professional/pediatrics/neurologic-disorders-in-children/cerebral-palsy-cp-syndromes. Accessed April 2022.
- Ng J, et al. Nat Rev Neurol. 2015;11:567–584.
- Kurian MA, et al. Lancet Neurol. 2011;10:721–733.
- Hallman-Cooper JL, Gossman W. StatPearls. Treasure Island, FL: StatPearls Publishing; 2019. Available at: https://www.ncbi.nlm.nih.gov/books/NBK538147/. Updated July 18, 2019. Accessed April 2022.
- Zouvelou V, et al. Eur J Paediatr Neurol. 2019;29(3):427–437.
- Manegold C, et al. J Inherit Metab Dis. 2009;32:371–380.
- Wassenberg T, et al. Orphanet J Rare Dis. 2017;12:12.
- Gururaj AK, et al. Seizure. 2003;12:110–114.
- Singhi P, et al. J Child Neurol. 2003;18:174–179.
Explore interactive clinical case studies
